Improve Cancer Immunotherapy by Reducing Toxicity of Lipid Nanoparticles
Chemotherapy is a cornerstone in cancer treatment, but its efficacy is often limited by adverse effects on the immune system. While chemotherapy can stimulate antitumor immunity, it may also impair immune cell function and induce lymphodepletion, reducing effectiveness of subsequent immunotherapy. Researchers constantly seek to strike a delicate balance between efficacy and safety and to mitigate these side effects. Nanoparticle-based drug delivery systems have been developed for its improved drug biodistribution and reduced toxicity. And combinatorial approaches involving nanoparticles and immunotherapy are now being explored extensively. However, the interaction between nanoparticles and immune system, particularly the formation of protein corona on nanoparticle surfaces, remains unclear.
Protein corona, composed of endogenous proteins adsorbed onto nanoparticle surfaces, can significantly alter the biological fate of nanoparticles. Apolipoproteins, such as ApoE and ApoA-1, are commonly enriched in protein corona of lipid nanoparticles and play crucial roles in modulating nanoparticle-cell interactions. ApoA-1, a natural ligand of scavenger receptor class B type 1 (SR-B1), has received little attention in nanoparticle-mediated chemotherapy, and its effects on immune responses remain unclear. High-density lipoprotein (HDL) is a natural nanoparticle containing ApoA-1. Via binding with SR-B1, HDL mainly transports hydrophobic cargo directly into the cytosol in an endocytosis-independent pathway, while the ApoA-1 remains in circulation and finally undergoes degradation in the kidney. Recently, synthetic HDLs (sHDLs) composed of ApoA-1 mimic peptides have been explored, resembling natural HDL in biocompatibility and SR-B1-based cell specificity. Though of different origins, both natural HDLs and sHDLs show capability of regulating innate immune responses.
In a study published in Science Advances on June 5, a research team led by LI Yaping from Shanghai Institute of Materia Medica (SIMM) of the Chinese Academy of Sciences, ZHANG Pengcheng from ShanghaiTech University, along with WANG Hao from China State Institute of Pharmaceutical Industry and other collaborators, revealed that ApoA-1 can transport drugs encapsulated within lipid nanoparticles to myeloid cells, leading to myelopenia and consequently lymphopenia. They demonstrated that these side effects can largely be avoided simply by conjugating drugs to the nanoparticles, without reducing antitumor activity of the drugs.
To investigate the influence of ApoA-1 on the immune response, researchers created two variants of maytansine (DM1)-loaded synthetic high-density lipoproteins (D-sHDL) with either physically entrapped (ED-sHDL) or chemically conjugated to ApoA-1 (CD-sHDL) DM1. By comparing their cell uptake mechanism, biodistribution, in vivo efficacy, and safety, researchers found that CD-sHDL showed less accumulation in the tumor-draining lymph nodes (DLNs) and femur. This resulted in lower toxicity against myeloid cells than ED-sHDL via avoiding SR-B1-mediated DM1 transportation into granulocyte-monocyte progenitors and dendritic cells. Therefore, higher densities of lymphocytes in tumors, DLNs, and blood were recorded in mice receiving CD-sHDL, leading to better efficacy and immune memory of CD-sHDL against colon cancer. Furthermore, liposomes with conjugated DM1 (CD-Lipo) showed lower immunotoxicity than those with entrapped drugs (ED-Lipo) through the same mechanism after apolipoprotein opsonization.
Given high translational potential of the two investigated lipid nanoparticles (sHDL and liposome) and prevalence of ApoA-1 as a main component of the protein corona, these findings shed light on designing nanoparticle-based chemotherapy strategies by elucidating the role of ApoA-1 in modulating immune responses. This study also deepens our understanding of the immune interaction of nanoparticles. Figuring out the complex interplay between nanoparticles and immune system will pave the way for development of more effective and less toxic cancer therapies in the future, and will impact on the clinical translation of nanoparticles for immune manipulation.
DOI: 10.1126/sciadv.adk9996
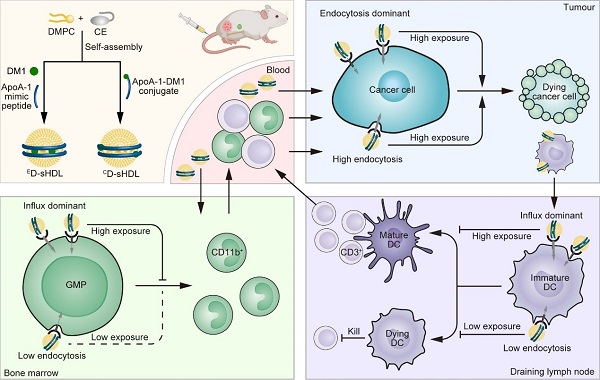
Schematic illustration of sHDL preparation and different impact on toxicity and efficacy of drug loading patterns in sHDL. DM1 is loaded into sHDL through either encapsulation or conjugation as illustrated to form ED-sHDL or CD-sHDL, respectively. After intravenous injection, DM1 that is physically encapsulated in ED-sHDL tends to be transported into GMP and DC through SR-B1-mediated influx and accumulate in bone marrow and draining lymph nodes, leading to myelotoxicity, lymphotoxicity, and antitumor immunity suppression. In contrast, DM1 that is conjugated to ApoA-1 in CD-sHDL can only enter cells through SR-B1-mediated endocytosis, which is a dominant internalization pathway in tumor cells but not in GMP and DC, ensuring efficient antitumor immunity activation while avoiding immunotoxicity. Cholesterol (CE), Dendritic cell (DC), Dimyristoylphosphatidylcholine (DMPC), Granulocyte-monocyte progenitor (GMP). Created with BioRender.com. (Image by ZHENG Chao)
Contact:
JIANG Qingling
Shanghai Institute of Materia Medica, Chinese Academy of Sciences
E-mail: qljiang@stimes.cn




